Unraveling the Twists and Turns of Lower Limb Claudication
Lower limb claudication is a condition that many in the medical community have encountered, yet its diagnosis and treatment can be riddled with tension and confusing bits. As an editor who explores both modern medicine and alternative approaches, I have been intrigued by recent cases that highlight the coexistence of both spinal and vascular contributors to this condition. In essence, lower limb claudication can be viewed as the result of multiple overlapping problems, and it is essential that clinicians take a careful, systematic approach to properly figure a path through these challenging presentations.
In many instances, the main causes of claudication have been traditionally compartmentalized into neurogenic and vascular origins. However, the case we are examining today demonstrates that these issues are not mutually exclusive. An intricate interplay of degenerative changes in the spine can occur in tandem with arterial stenosis in the lower limbs. As modern imaging techniques become more advanced, a clearer picture emerges—one that forces us to embrace a dual diagnosis when the clues point to an overlap between spinal canal stenosis and impairments in arterial circulation.
Identifying the Dual Aetiology: Spinal and Vascular Overlap
One of the trickiest parts in lower limb claudication is making sense of the overlapping symptoms that share a common root. In a recent report concerning a 60-year-old male with a background of coronary artery disease, the symptoms ranged from persistent lumbosacral back pain to progressive bilateral leg claudication. The patient’s history, marked by significant cardiovascular risk factors including smoking and dyslipidemia, suggested vascular issues at first glance. However, careful imaging revealed a lumbar facet joint synovial cyst that was compressing the spinal canal.
This dual scenario—a spinal pathology coupled with critical bilateral femoral artery stenoses—teaches us several key lessons:
- The importance of thorough clinical assessment: A superficial clinical evaluation might drive a clinician to attribute the symptoms solely to vascular claudication, especially in patients with an extensive cardiovascular history.
- The necessity for multiple diagnostic tools: Combining MRI for spinal issues with CT angiography for vascular mapping can help uncover the hidden complexities in a patient’s condition.
- A staged intervention strategy: Addressing the spinal component first, followed by vascular treatment, can lead to a full resolution of symptoms while mitigating risk.
When both spinal and vascular elements are present, the challenge of diagnosing the true source of discomfort becomes a series of steps rather than a one-shot evaluation. It is crucial to remain open to the possibility of dual pathology, particularly in older patients who have a blend of risk factors for both degenerative and atherosclerotic disease.
Tackling the Tricky Parts of Diagnosing Combined Pathologies
Diagnosing dual pathology involves grappling with a number of confusing bits that might easily be misinterpreted. The symptoms between neurogenic and vascular claudication may overlap, and clinicians must be guided by both the patient’s history and subtle clinical cues. For instance, neurogenic claudication tends to improve when the patient adopts positions that flex the spine, such as sitting or squatting; in contrast, vascular claudication is typically exercise-induced and resolves with rest.
However, when both types of pain are present, the differentiation becomes a nerve-racking process. The following factors are key when sorting out the overlapping clinical pictures:
- Symptom timing and relief patterns: Noting how symptoms change with activities can provide insights. A patient who experiences immediate pain relief with a change in posture hints at a neurogenic component, whereas persistent pain after minimal exertion might indicate vascular compromise.
- Anatomical imaging: High-resolution imaging such as MRI and CT angiography plays an essential role in delineating the fine points of the pathology. These modalities help identify a synovial cyst in the facet joint or critical stenosis in the femoral arteries.
- Risk factor correlation: Understanding the patient’s overall risk profile—such as long-term smoking, high alcohol consumption, and a history of coronary interventions—can guide the clinician in weighing both causes equally.
Moreover, as medicine advances, there is a growing recognition that anchoring on a single causative factor is a dangerous oversimplification. Instead, sorting out the subtle differences and making use of detailed patient history, combined with multiple imaging studies, provides a clearer diagnostic picture.
Innovative Minimally Invasive Interventions in Modern Healthcare
Modern healthcare has witnessed a significant shift towards minimally invasive procedures that aim to reduce recovery time, lower the risk of complications, and avoid the need for open surgery. The case discussed earlier is a prime example of how sequential, percutaneous interventions can resolve symptoms completely.
In the described case, the patient first underwent a CT-guided percutaneous injection to address the lumbar facet joint synovial cyst. This procedure, which involved rupturing the cyst under image guidance, resulted in partial relief—specifically alleviating the neurogenic claudication symptoms. However, the vascular concerns remained, and those issues were addressed later by percutaneous transluminal angioplasty (PTA). The staged approach demonstrated that by dealing with each pathology individually, one can achieve complete symptom resolution with minimal invasiveness.
Key advantages observed with these interventions include:
- Reduced procedural risk: Minimally invasive treatments decrease the risk of complications like infection or prolonged recovery associated with open surgery.
- Shorter hospital stays: Patients typically experience less downtime and can return to daily activities, such as farming in this case, much more quickly.
- Improved precision: Image-guided techniques allow for exact targeting of the pathology, whether it is through a spinal injection or an endovascular procedure.
This case demonstrates how, with the advancement of modern radiological techniques, clinicians can manage the tangled issues that arise from dual pathology in a safe and effective manner. It is a reminder that the combined use of imaging and a staged treatment strategy is not only practical but also often necessary when confronted with atypical cases.
A Closer Look at Stepwise Management Strategies
The successful treatment of dual pathology in this scenario underscores the importance of taking a stepwise approach when faced with multiple contributing factors. The sequence of interventions was determined by the severity of symptoms and the patient’s primary complaint. Initially, the patient’s overwhelming neurogenic pain—characterized by lower back pain radiating to the gluteal region—required urgent effective management. After the CT-guided injection produced partial relief, the patient was left with persistent vascular claudication that limited his ambulation.
The subsequent intervention consisted of careful, staged PTA of the affected femoral arteries. The procedure was performed first on the right side, which showed more severe compromise, followed by corresponding treatment on the left. In this way, each intervention built upon the last, contributing cumulatively to full recovery. This step-by-step method makes it easier for clinicians to assess the individual impact of each treatment and adjust the management plan accordingly.
Some strategies for successful stepwise management include:
- Prioritizing interventions: Determine which pathology is contributing most significantly to the patient’s symptoms and address that component first.
- Monitoring in between stages: Allow enough time between procedures to evaluate symptom improvement and adjust plans for subsequent interventions.
- Using clear imaging guidance: Maintain a reliance on detailed radiological assessments to guide both the decision-making and the technical aspects of the interventions.
Overall, the layered approach used in these types of cases provides a model for how modern medicine can deal with multifactorial presentations in a way that reduces risk and improves outcomes without immediately resorting to more invasive surgical options.
The Crucial Role of Imaging in Sorting Out Overlapping Causes
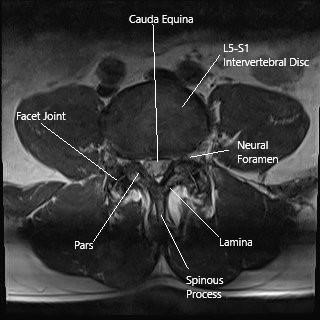
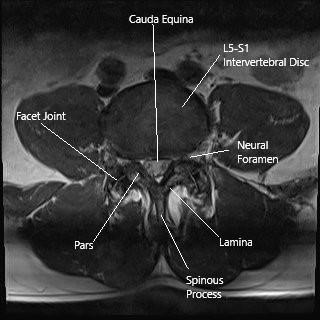
Modern imaging techniques have revolutionized the ability to pinpoint both obvious and hidden issues. For patients with suspected lower limb claudication, MRI stands as the gold standard for exploring spinal degeneration, including conditions such as lumbar facet joint synovial cysts. These cysts form due to degeneration of the facet joint and may impinge on the spinal canal, triggering neurogenic pain.
CT angiography, on the other hand, provides a clear picture of the vascular system. Its high-resolution capabilities allow clinicians to identify precise locations and the severity of arterial stenoses, such as those affecting the common and superficial femoral arteries. In combining these imaging modalities, healthcare providers are better equipped to figure a path through the multiple layers of pathology.
Utilizing imaging effectively involves:
- Early detection: Identifying subtle structural changes in the spine before they lead to significant neurological deficits.
- Precise mapping: Generating detailed vascular maps which help in planning the optimal route for interventions like PTA.
- Follow-up monitoring: Repeating imaging studies after intervention to assess the long-term success of the treatment, ensuring that no further issues have arisen post-procedure.
When health professionals combine these imaging techniques, they are not only managing to get a clearer look at the fine shades of the pathology but also paving the way for a tailored treatment plan that minimizes unnecessary risk and maximizes patient outcomes.
Patient Experience and Clinical Outcomes
Beyond the technical merits of sequential radiological interventions, the real measure of success is seen in patient outcomes and overall quality of life. In the case of the 60-year-old male farmer, the drastic improvement in his symptoms translated into a restored ability to work and engage in daily activities without discomfort. The partial improvement observed after the CT-guided injection paved the way for further intervention on the vascular front, leading to a complete resolution of his symptoms.
This outcome is supported by various clinical studies. For example, retrospective analyses have shown that CT-guided injections for lumbar facet joint synovial cysts have offered symptom relief in over half of treated patients, reducing the need for open or more invasive surgical interventions. In parallel, staged PTA procedures have consistently demonstrated improvements in walking distance and overall limb function in patients diagnosed with peripheral arterial disease.
In clinical practice, such layered management not only resolves the immediate issues but also has several secondary benefits:
- Minimizing complications: By avoiding large-scale surgical interventions, patients are less likely to experience complications such as infection, prolonged rehabilitation, or other perioperative issues.
- Targeted therapy: A staged approach allows clinicians to adjust the treatment plan based on the patient’s response at each step, thus ensuring that the intervention remains aligned with the evolving clinical picture.
- Improved quality of life: Ultimately, the goal is to help patients return to their baseline level of function, as evidenced by our patient who resumed his farming activities and achieved an impressive ambulation distance post-treatment.
This kind of patient-centered approach embodies the delicate balancing act required in modern healthcare, where the aim is not merely to treat a disease but to restore functional independence and well-being.
Managing Your Way Through the Challenging Landscape of Dual Pathology
For clinicians, the case of coexisting lumbar facet joint cyst and critical arterial stenoses is a reminder of the tricky parts involved in diagnosing multifactorial conditions. It is all too easy to be overwhelmed when symptoms seem to pull in different directions. However, by taking a closer look at each component and managing the treatment step by step, the medical team in our examined case was able to make their way through the tangled issues with remarkable precision.
The following checklist offers a practical guide for healthcare professionals when faced with similar dual pathologies:
| Step | Action | Outcome |
|---|---|---|
| 1 | Conduct a detailed patient history and physical examination | Identify potential risk factors and symptom patterns |
| 2 | Utilize multimodality imaging (MRI and CTA) | Differentiate between neurogenic and vascular contributors |
| 3 | Prioritize treatment based on the severity of symptoms | Implement a staged treatment plan |
| 4 | Monitor patient response after each intervention | Adjust further interventions if necessary |
| 5 | Follow up with imaging and clinical evaluations | Ensure long-term success and functionality |
The table above highlights the key steps and outcomes that can help guide clinicians when the patient’s presentation includes both neurogenic and vascular elements. It reinforces the importance of having not just one but multiple strategies to work through these nerve-wracking issues.
Innovative Perspectives on Minimally Invasive Radiological Treatments
In recent years, there has been a growing movement towards incorporating less invasive interventions in the treatment algorithms for complex conditions. The combination of CT-guided facet joint cyst rupture and percutaneous transluminal angioplasty (PTA) demonstrates a forward-thinking approach that balances efficacy with the comfort and safety of the patient.
This innovative strategy offers several benefits:
- Precision: Both procedures are guided by high-resolution imaging, enabling the clinician to target the affliction directly with minimal collateral damage.
- Efficiency: A staged approach allows for individual assessment after each intervention, ensuring that each step is effective before moving to the next.
- Reduced stress on the patient: Minimally invasive techniques typically result in less postoperative discomfort and faster mobilization.
Although the dual treatment scenario was unusual, the outcomes underline the critical fact that, when performed in appropriate sequence, such interventions can collectively overcome the challenges posed by full-scale open surgery. In many ways, these procedures reflect the evolving nature of modern medical interventions, where the focus is not solely on immediate correction but on long-term functional recovery.
Implications for Future Healthcare and Clinical Practice
The lessons learned from this dual-pathology case offer promising insights for the future of clinical practice. In a world where the aging population is increasingly likely to present with multiple overlapping conditions, clinics and hospitals must prepare for a landscape that is full of problems and twisted complexities.
Some implications of adopting a dual diagnostic and therapeutic strategy include:
- Enhanced interdisciplinary collaboration: Successful management of multifactorial conditions demands close coordination between radiologists, vascular surgeons, and spine specialists. This encourages a team-based approach to patient care, where expertise is pooled to handle the interlocking challenges.
- Increased reliance on advanced imaging: As we have seen, obtaining detailed, high-quality images is indispensable in teasing apart the fine shades that distinguish neurogenic from vascular contributions. Future advancements in imaging technology could further streamline diagnosis and treatment planning.
- Personalized treatment planning: Each patient’s clinical scenario is unique. Treatment protocols that allow for adjustments based on patient response will become more widespread, fostering individualized healthcare that moves away from one-size-fits-all approaches.
- Optimization of resource allocation: Minimally invasive procedures, while technologically demanding, tend to reduce overall hospital stay and recovery time. This not only alleviates patient burden but also improves the efficiency of healthcare systems by freeing up critical resources for other patients in need.
These implications create a promising vision for healthcare that is better equipped to deal with the tangled issues of combined pathologies. Integrating modern imaging and minimally invasive techniques into a clear, staged treatment protocol is a super important evolution in patient care that is set to improve outcomes and enhance quality of life.
Balancing Risks and Rewards in a Dual-Treatment Approach
No medical intervention is without its risks, and the dual treatment approach for claudication is no exception. There are certain nerve-wracking factors that must be taken into account when planning and executing these procedures. For instance, potential complications from percutaneous interventions might include bleeding, infection, or contrast-induced nephropathy in vulnerable patients with preexisting conditions.
However, the rewards of a careful and staged approach can far outweigh these concerns when executed properly. Some of the strategies for managing these risks include:
- Pre-procedure evaluation: Detailed medical histories, comprehensive blood work, and rigorous imaging studies help clarify the patient’s risk profile.
- Using minimal contrast dosing: Contemporary practices in interventional radiology use advanced contrast dosing guidelines which minimize renal stress and other side effects.
- Post-intervention monitoring: Close follow-up and serial assessments ensure that any complications are identified early and managed effectively.
This balance between risk and reward requires clinicians to be adaptive. By acknowledging the possible pitfalls and then planning procedures accordingly, it is possible to overcome the intimidating aspects that come with managing dual pathologies.
Learning from Real-World Experiences
In my long years of tracking advancements in healthcare, I have observed that real-world experiences often serve as the best teacher. The case of the 60-year-old farmer is a prime example of this, where the spine and vascular systems both contributed to a patient’s debilitating symptoms. Ultimately, the staged, minimally invasive interventions not only provided symptom relief but also offered a framework from which future cases can draw inspiration.
The lessons gleaned from such experiences include:
- Curiosity and open-mindedness: Clinicians must remain open to the idea that more than one pathology may be present, even if initial evidence points to a singular cause.
- Vigilance in monitoring: Regular follow-up assessments using clinical evaluation and imaging allow healthcare providers to track improvement and ensure long-term success.
- Patient-centric care: In the end, the measure of success is whether the patient can return to normal activities—be it walking a couple of hundred meters or going back to work without pain.
By poking around the fine details and nurturing a mindset that is receptive to multiple interpretations, clinicians can better sort out the tangled issues inherent in such dual pathology cases. It is this blend of curiosity, technical expertise, and disciplined follow-up that will serve as the cornerstone for future advancements in managing lower limb claudication.
Conclusion: Embracing the Full Spectrum of Diagnostic and Therapeutic Options
Lower limb claudication, whether stemming from neurogenic or vascular origins, is a condition replete with tricky parts and tangled issues that demand a nuanced and careful approach. The case of coexisting lumbar facet joint synovial cyst and critical femoral artery stenoses illustrates vividly how early detection, advanced imaging, and sequential minimally invasive interventions can collectively resolve what might otherwise be a nerve-wracking scenario.
This experience serves as a strong reminder that systematic and stepwise management is not just a theoretical ideal but a practical necessity. By working through each intervention methodically—first addressing the spinal component and then tackling the vascular insufficiency—clinicians can achieve excellent outcomes while sparing patients from the risks of open surgery.
Furthermore, this case highlights the growing role of imaging in modern diagnostics. With MRI and CT angiography providing invaluable insights into the fine points of pathology, radiology has become an indispensable partner in diagnosing and treating dual pathologies. As technological advancements continue, the precision and efficacy of these diagnostic tools will only enhance the quality of patient care.
For both clinicians and patients, the key message is clear: when faced with overwhelming, dual-layered symptoms, it is essential to keep an open mind, use every tool available, and consider a staged treatment approach. In doing so, we not only resolve the immediate symptoms but also pave the way for a more sustainable, longer-term recovery.
Ultimately, as our patient’s story shows, thinking beyond conventional diagnostic boundaries and embracing a flexible, patient-centered treatment plan can result in complete restoration of function and an improved quality of life. It is this philosophy—grounded in advanced imaging, minimally invasive procedures, and multidisciplinary collaboration—that will shape the future of modern healthcare when it comes to treating lower limb claudication and similar conditions.
In conclusion, when we take the time to figure out the subtle details and work through the intimidating twists and turns of dual pathology, we empower ourselves to deliver care that is both effective and compassionate. As we continue to innovate and refine our approaches, the hope is that more patients will benefit from treatments that not only address the symptoms on the surface but also tackle the underlying causes with precision and care.
Originally Post From https://www.cureus.com/articles/403957-dual-aetiology-of-lower-limb-claudication-a-rare-case-of-coexisting-lumbar-facet-joint-synovial-cyst-and-critical-lower-limb-arterial-stenoses
Read more about this topic at
Effective Strategies for Managing Dual Diagnosis
Chapter 5—Strategies for Working With People Who Have …