Capitation Payment Takes the Wheel: A New Direction in Diabetes Care
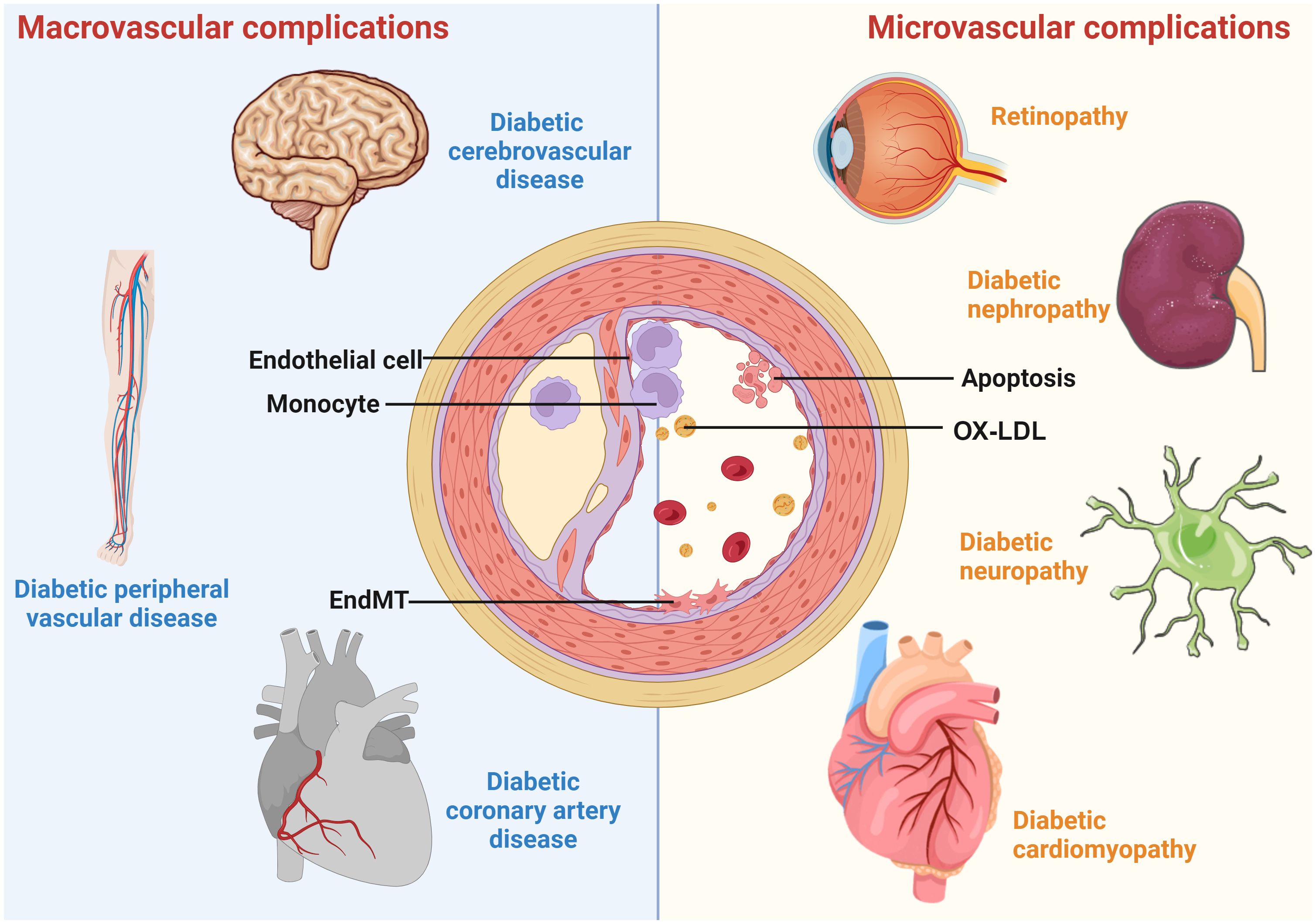
The recent wave of healthcare reforms in China has sparked an intriguing debate about how capitation payment models could steer improvements in the management of diabetes. In a far-reaching study from Tianjin, researchers have examined how switching from traditional fee-for-service to a capitation model might reduce the occurrence of vascular complications among diabetic patients. This opinion editorial takes a closer look at the findings, examines the subtle parts of the payment reform, and digs into the potential long-term effects on patient outcomes.
Diabetes, with its tangled issues and complicated pieces, has long challenged health systems worldwide. Policymakers and healthcare professionals have wrestled with both the tricky parts of controlling costs and ensuring high-quality care. The study in question shines a light on one innovative approach—capitation payment, a method that provides a fixed amount per patient rather than reimbursing individual services. This approach creates an environment where healthcare providers are encouraged to optimize resources, manage patient care more holistically, and potentially lower the incidence of severe complications.
Unpacking the Capitation Payment Model: The Fine Points and Hidden Complexities
Capitation payment can appear intimidating at first glance due to its many twists and turns. Unlike fee-for-service, where hospitals and clinicians are paid for each service rendered, capitation offers a pre-determined amount, incentivizing cost control and a more careful allocation of resources. Naturally, there are some confusing bits:
- Budget Management: Providers must figure a path to deliver care within a strict budget, often requiring a detailed review of existing procedures and a willingness to shift from routine practices.
- Behavioral Adaptations: Doctors may change how they engage with patients, such as moving from frequent in-person visits to using remote monitoring tools.
- Risk of Under-Service: There is a concern that the drive for cost savings might lead to fewer diagnostic checks or less intensive treatment in some cases.
Yet, it is precisely this separation between direct service payment and overall patient care that has the potential to yield significant improvements in the management of chronic diseases like diabetes. By reworking these tangled issues, healthcare providers might be able to deliver more streamlined and focused care, albeit with the risk of encountering nerve-racking trade-offs.
Evidence from Tianjin: A Quasi-Natural Experiment in Payment Reform
A groundbreaking study from Tianjin serves as a testimony to the potential benefits of capitation payment in reducing vascular complications among diabetic patients. Conducted as a quasi-natural experiment, the research compared two distinct groups: one that embraced the capitation payment model and a control group that stuck with the traditional fee-for-service approach. The study spanned over eight years and carefully matched 23,258 patients to ensure a fair comparison between the groups.
Key findings of the study included:
- Notable reductions in the incidence of peripheral neuropathy, diabetic foot, and cardiovascular diseases when compared with patients under fee-for-service.
- A steady decline in complication rates over time, suggesting a learning effect on the part of the healthcare providers.
- Subgroup analyses revealing that retired patients, in many cases, experienced even lower complication rates compared to currently employed patients.
These results indicate that the capitation model not only contains costs but also offers super important improvements in patient safety and overall health outcomes—a win-win that prompts us to take a closer look at what really drives quality care in chronic disease management.
Examining the Learning Curve: When Improvements Take Time to Unfold
The study’s results remind us that improving the delivery of healthcare is not an overnight achievement. Instead, it involves sorting out several long-term factors and subtle details that may only reveal themselves as experience and practice accumulate. During the first two years after capitation implementation, some macrovascular complications such as peripheral vascular disease and cardiovascular disease did not display as significant a change. However, as time went on, the data showed a noticeable drop in complications—especially in the areas of diabetic foot, diabetic nephropathy, and retinopathy.
This lag in observable benefits can be understood as a learning curve. Healthcare providers needed time to adapt their practice styles, adjust diagnostic criteria, and find new ways of engaging with patients to manage chronic conditions effectively. Once these fine shades of operational change took hold, the results became more pronounced, suggesting that capitation payment may require a period of adjustment before its benefits are realized.
Detailed Analysis: Getting into the Numbers
A careful reading of the study’s tables and statistical analyses reveals a number of interesting points. For instance, the researchers used a rigorous approach—combining Propensity Score Matching (PSM) with Difference-in-Differences (DID) regression—to control for potential biases and ensure that the findings were truly reflective of differences in payment methods rather than patient selection factors.
| Complication Type | Odds Ratio (Capitation vs Fee-for-Service) | 95% Confidence Interval |
|---|---|---|
| Peripheral Neuropathy | 0.900 | 0.862 to 0.941 |
| Peripheral Vascular Disease | 0.758 | 0.726 to 0.792 |
| Diabetic Nephropathy | 0.723 | 0.689 to 0.758 |
| Retinopathy | 0.754 | 0.721 to 0.789 |
| Cardiovascular Disease | 0.629 | 0.601 to 0.657 |
| Diabetic Foot | 0.522 | 0.490 to 0.557 |
By analyzing these numbers, it is apparent that patients under the capitation payment model had a significantly lower risk—often by more than 20% to 40%—of developing various complications. The detailed breakdown helps illustrate that while every system comes with its tangled issues, a well-managed capitation model can help healthcare providers find ways to overcome these challenges over time.
A Closer Look at Patient Subgroups: Employed Versus Retired
One of the more interesting facets of the study was an analysis that considered patient retirement status. This subgroup analysis digs into the fine points of how capitation payment models affect different populations. The researchers discovered that the incidence of vascular complications was generally lower among retired individuals than among employed ones in the capitation group. Here are a few reasons that might help us understand this difference:
- Higher Capitation Fees: Retired patients often received a higher capitation fee, which could empower hospitals and physicians to allocate more resources per patient.
- Lower Disease Awareness: Retired individuals may undergo fewer diagnostic procedures, which sometimes correlates with a reduced incidence of over-diagnosed complications.
- Socioeconomic Factors: Employed individuals, often tied to higher socioeconomic status, might engage in different health-seeking behaviors that influence treatment decisions.
- Adherence to Treatment: Retirees might have more time and energy to stick to treatment plans, thereby lowering their risk of severe complications.
These findings suggest that capitation payment models are nuanced and that the subtle differences in how they affect various patient groups are crucial to understanding the overall benefits and potential limits of such reforms.
Future Implications: Steering Through Policy and Practice
As we work our way through the challenges of modern medicine, it is critical to consider the broader implications of payment reforms like capitation. The Tianjin study is on edge in several ways: it demonstrates that changes in physician practices, when aligned with appropriate financial incentives, can bring about measurable improvements in patient outcomes. But it also comes with caveats. Implementation is not without its nerve-racking fine points, such as the need to ensure that cost-saving measures do not compromise care quality.
For policymakers and healthcare administrators, these findings prompt several key considerations:
- Budget Allocation: The fixed fee per patient must be thoughtfully set based on regional differences and patient demographics to avoid overwhelming providers with a nerve-racking budget shortfall.
- Training and Education: Physicians require support to adopt innovative, non-visit-based care models. Continued education and investment in digital monitoring tools or remote consultation platforms can help bridge the gap in the early, intimidating stages of implementation.
- Monitoring and Feedback: Establishing robust oversight and reporting systems is super important to continuously evaluate the model’s performance and address any head-scratching issues as they arise.
- Patient-Centered Care: Ensuring that the model truly improves health outcomes requires integrating patient feedback, particularly from vulnerable groups such as the elderly or those with multiple chronic conditions.
These points suggest that while capitation payment models could be a transformative force in managing chronic diseases like diabetes, they are loaded with potential pitfalls. Taking the time to carefully implement, monitor, and adjust these systems is a must-have strategy to ensure that the cost-savings do not come at the expense of patient care.
Digging into the Changing Landscape of Chronic Disease Management
The healthcare industry is continuously evolving, and the emergence of capitation payment models represents a strategic shift in how care is delivered and financed. When traditional systems struggle under the weight of high expenditures, innovative solutions emerge that allow providers to make your way through the challenging parts of managing chronic illnesses.
Capitation payment can influence various facets of care delivery, such as:
- Preventive Care: With a fixed payment framework, doctors may feel more inclined to invest in preventative measures, ensuring that complications are caught early on before they spiral into severe conditions.
- Remote Monitoring: The drive to manage care within a fixed budget encourages the use of telemedicine and remote monitoring technologies that help reduce the need for expensive, in-person visits.
- Patient Education: A big part of diabetes management involves lifestyle changes. By ensuring that patients are well-informed and actively engaged with their healthcare providers, capitation models can promote long-term positive behavioral shifts.
While these adjustments may seem like small distinctions at first, they represent small twists that can lead to improvements in overall care quality. In an environment where each decision counts, the ability to pivot from reactive to proactive care is an essential evolution in modern medicine.
Potential Pitfalls: The Hidden Risks of Capitation Payment Models
No policy model is without its tricky parts, and capitation is no exception. Among the possible concerns are the risks that providers might shortchange necessary care in a bid to adhere to budget limits. Critics of this approach often point out several nerve-racking areas that must be managed:
- Under-Service Risk: There may be a temptation to reduce the number or quality of services provided to maximize financial surplus, which in turn might lead to patients missing out on crucial diagnostics or therapies.
- Provider Burnout: When healthcare providers are pressured to stay within rigid budgets, the hectic balancing act can be overwhelming—adding stress to an already demanding profession.
- Patient Selection Bias: Although the Tianjin study took care to address this issue, there is always a concern that providers and insurers might subtly steer patients toward or away from a particular payment method based on underlying health needs, rather than clinical criteria alone.
These points might feel a bit overwhelming, but they remind us that the process of modernizing payment systems is on edge with inherent uncertainties. It is vital to poke around for solutions that protect both providers and patients. A well-structured oversight process, transparent communication channels, and robust data collection systems are super important for mitigating these risks.
Personalizing Payment Models for Better Outcomes
The varied experiences observed between retired and employed patients in the study illustrate that a one-size-fits-all approach might not be optimal. Instead, refining capitation payment models with an eye to personalizing care could yield improvements in how providers steer through these complicated pieces.
For example, adjustments such as differential capitation fees based on patient demographics and medical history could lead to better outcomes. The study found that retired patients, who often have higher capitation fees, tended to enjoy lower rates of complications. This insight points to the intrinsic value of tailoring financial models to account for different patient needs and risk profiles.
Such personalized approaches might include:
- Customized Budgeting: Crafting different capitation rates for subgroups—such as separating individuals by age group, employment status, or overall health status—could help ensure that all patients receive the level of care they require.
- Integrated Care Teams: Encouraging collaboration among doctors, nurses, and other healthcare professionals can help create more comprehensive care plans that address the multiple facets of diabetes management.
- Enhanced Data Analysis: Regularly reviewing patient data to fine-tune payment rates and care protocols can help identify which elements of the capitation model are working best and which need adjustment.
This strategy, if taken to heart, has the potential to transform the capitation model from a blunt financial tool into a finely honed instrument of patient-centered care.
Engaging Multiple Stakeholders in the Reform Process
Implementing capitation payment models involves more than just making changes from the boardroom. To truly effect positive change, a wide array of stakeholders must be involved—from policymakers and healthcare providers to patients themselves. Each group brings a unique perspective to the table, offering valuable insights into how to best manage the nerve-wracking parts of implementation.
Stakeholder engagement is key in addressing several central issues:
- Clinical Input: Doctors and nurses have firsthand experience of the daily challenges of diabetes management. Their feedback can help refine capitation models to better fit real-world clinical scenarios.
- Patient Voices: Ensuring that patients understand the new payment model and feel confident in their care is super important. Clear communication about how these changes affect their treatment can ease concerns and encourage active participation.
- Policy Guidance: Government agencies and insurance bodies provide the regulatory framework that underpins these reforms. Working together to set clear standards and monitor outcomes is critical to success.
In practice, this means regular consultations, transparent reporting of outcomes, and ongoing training sessions for all involved parties. By creating a collaborative ecosystem, the healthcare system can better manage the tricky parts of transitioning to a capitation-based approach.
Steps Forward: Evaluating the Model’s Impact Amid Ongoing Reforms
As with any significant change, evaluating the effectiveness of capitation payment models will require continuous monitoring and periodical reassessment. The Tianjin study offers a detailed set of benchmarks that can serve as a foundation for broader analysis. Future research may focus on:
- Long-Term Outcomes: Tracking patient health outcomes over a longer period can give a more complete picture of how capitation impacts the progression of diabetic complications.
- Cost-Efficiency Analysis: Evaluating how much money is saved while ensuring that patient care remains uncompromised is a critical area of future inquiry.
- Comparative Studies: Comparing capitation models across different regions or patient groups may help identify the small distinctions that lead to superior care practices.
These research efforts are essential in ensuring that the system continues to evolve in a manner that balances cost control with quality improvements. In a healthcare environment replete with ambiguous bits and tangled issues, evidence-based adjustments are the key to forging a path forward.
Lessons for Global Health Policy: Transferring Insights Beyond China
While the current study focuses on a specific region in China, its implications resonate with global healthcare systems grappling with the growing burden of chronic diseases like diabetes. Many countries are exploring alternatives to fee-for-service payment models in an effort to contain rising healthcare costs without compromising the quality of care.
Some key lessons in the context of international health policy include:
- Adapting to Local Needs: Each country has its own cultural, economic, and clinical settings. Therefore, while the capitation model shows promise, its implementation must be adapted to the local context.
- Collaborative Learning: Countries can benefit from sharing their experiences, both the successes and the nerve-racking challenges. International conferences and collaborative research can serve as catalysts for innovation.
- Balancing Act: The emphasis should remain on finding your way through both cost containment and quality care. Global health systems must take the time to figure out how to maintain a balance that does not sacrifice the well-being of patients for economic efficiency.
These points underscore the broad potential of capitation payment models. Though there are tricky parts and potential pitfalls, countries around the world may find that these models help to streamline care, reduce unnecessary spending, and promote patient-centered service delivery.
Reflecting on the Broader Impact: A Call for Patient-Centric Reforms
Ultimately, the debate over payment models is a proxy for a larger conversation about the future of healthcare. At its core, this discussion revolves around the question: How do we design systems that not only curb cost escalation but also deliver super important improvements in patient outcomes?
The Tianjin study reminds us that balancing these goals is a masterful act of managing your way through a labyrinth of competing interests. It calls for a pragmatic approach where healthcare providers, policymakers, and patients work together to streamline clinical practices, invest in preventative care, and ultimately reduce the burden of complications in chronic disease management.
Among the key takeaways, our discussion highlighted the following insights:
- The Need for Flexibility: Capitation models must be adaptable to the unique challenges posed by chronic diseases, such as the long-term nature of diabetic complications and varying patient demographics.
- Time as a Factor: Immediate results may not reflect the true benefits of the model. Patient outcomes improve gradually as physicians master new approaches, underscoring the need for sustained policy support and long-term monitoring.
- Personalized Approaches: Recognizing the distinct needs of subpopulations—such as retired versus employed patients—and adjusting payment rates and care protocols accordingly can further improve health outcomes.
- Collaborative Engagement: All stakeholders must be on board. From policymakers who shape the regulatory environment to clinicians on the front lines and patients who bear the brunt of chronic illness, everyone has a role to play in designing systems that work.
As healthcare systems worldwide face the daunting challenges of an aging population and rising chronic diseases, the insights from Tianjin may provide a roadmap for decreasing complications and improving overall quality of life. It is an invitation for countries to consider patient-centric reforms that can transform the way chronic diseases are managed.
Charting a New Course: Policy Recommendations and Future Directions
Given the evidence at hand and the multiple layers revealed by the study, several policy recommendations are emerging that could help guide future payment reform initiatives:
- Implement Gradually: Roll out capitation payment models incrementally to allow healthcare providers time to adjust to the new system. Continuous evaluation will help smooth out the initial nerve-wracking challenges.
- Increase Investment in Technology: Telemedicine services, remote monitoring systems, and health information exchanges are essential in supporting non-visit-based care—thus helping providers make your way through the tangled issues of chronic disease management.
- Tailor Payment Rates: Recognize that different patient groups have different needs. Adjusting capitation fees to reflect these differences—such as higher rates for retired individuals—could lead to better resource allocation and improved patient outcomes.
- Strengthen Clinical Guidelines: Develop and reinforce guidelines that prioritize preventive care and early intervention. These guidelines can help ensure that cost savings do not lead to under-service.
- Engage in Regular Training: Offer educational programs to assist medical staff in taking a closer look at new practices and integrating digital tools into their routine care strategies.
- Enhance Data Collection: Reliable, transparent data is crucial. Continuous monitoring and regular reporting will allow adjustments that address the inevitable slight differences that emerge over time.
These actionable recommendations reflect the super important need to manage not just the cost of care, but also its quality. In doing so, policymakers can work towards a model of care that is both cost-effective and patient-centered, reducing the complex twists and turns often associated with chronic disease management.
Conclusion: A Promising Yet Challenging Journey Ahead
The exploration of capitation payment models in diabetes care, as evidenced by the study from Tianjin, provides both optimism and caution. On one hand, the tangible reduction in vascular complications among diabetic patients under capitation highlights a promising path forward—one that aligns financial incentives with improved patient outcomes. On the other hand, the complex pieces and nerve-racking fine print remind us that transforming healthcare delivery involves managing many challenging parts.
As healthcare systems continue to evolve, the key is to maintain a balanced approach that does not sacrifice thorough, patient-centered care in the pursuit of cost containment. The experience in Tianjin teaches us that when providers have time to adapt, supported by incremental policy reforms and ongoing stakeholder engagement, substantial improvements in managing chronic conditions like diabetes are within reach.
In sum, the capitation payment system offers a fresh perspective on how we might rework healthcare financing to address both the economic and clinical challenges of chronic diseases. Its gradual, learning-driven implementation could pave the way for a healthier future where patients are less burdened by complications and healthcare providers can focus on delivering the best possible care. While questions remain and the journey is riddled with subtle challenges, the study serves as an essential step in reimagining a system where quality of care is as critical as managing costs—a truly patient-centric vision for the future of medicine.
Originally Post From https://www.nature.com/articles/s41598-025-17273-x
Read more about this topic at
The Future of Capitation: The Physician Role in Managing …
The Case for Capitation

