Exploring New Horizons in Coronary Interventions: A Closer Look at Repeated Stent-Less PCI for Calcified Nodules
The field of modern cardiology is constantly evolving, and recent advances in interventional techniques are opening up new possibilities for patients with complex coronary conditions. A case that has sparked significant discussion involves a 76-year-old male with recurrent restenosis caused by calcified nodules in the left circumflex artery. This opinion editorial takes a closer look at the repeated stent-free percutaneous coronary intervention (PCI) approach that utilizes aggressive debulking and drug-coated balloons (DCB) as a promising alternative for tackling these challenging lesions.
At first glance, the idea of repeatedly performing PCI without the use of permanent stents might seem daunting or even nerve-racking to some clinicians. However, careful consideration of the clinical outcomes, patient quality of life, and evolving technology suggests this approach deserves a closer look. In the following sections, we will dig into the underlying strategy, outline its underlying rationale, and review the benefits that may come from embracing repeated debulking methods in the face of persistent coronary lesions.
Understanding the Unique Challenges of Calcified Nodules in Coronary Artery Disease
Calcified nodules (CNs) present a set of tricky parts that make effective treatment a complicated endeavor. Unlike smooth, pliable blockages, these lesions involve hardened deposits in the arterial walls, which not only limit the ability of conventional balloon angioplasty to adequately dilate the vessel but also complicate the use of drug-eluting stents. The rough, uneven surface of calcified nodules can lead to suboptimal stent deployment, which in turn increases the chances of recurrent restenosis.
Reviewing these tangled issues, it is evident that an aggressive but careful strategy is needed. One novel approach involves performing repeated stent-less PCI with the aim of mechanically debulking the calcified tissue. By getting rid of as much calcification as possible, interventionists can then follow up with drug-coated balloon (DCB) angioplasty to deliver medication locally. This two-pronged approach is intended to control further restenosis while avoiding the complications that can arise with an implanted stent.
Repeated Aggressive Debulking: A Closer Look at the Technique
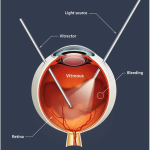
One of the key components of this innovative strategy is the repetitive use of aggressive debulking techniques. Atherectomy devices, when used correctly, can meticulously remove calcified deposits. This targeted removal is crucial, as it tackles the root of the problem, albeit through a process that is occasionally seen as off-putting due to its intensity. Nevertheless, once the bulk of the calcification is cleared, the application of DCBs plays an essential role in managing the vessel’s response.
It is important to recognize that the approach requires a thorough understanding of the small distinctions between various types of calcified lesions. The debate over whether repeated debulking might compromise vessel integrity is ongoing. However, case studies like the one under discussion reveal that with careful patient selection and precise technique, what initially appears to be a nerve-racking option can actually deliver sustained improvements in blood flow and reduce the frequency of restenosis over the long term.
Drug-Coated Balloons: A Modern Tool in the Interventional Cardiologist’s Arsenal
Drug-coated balloons (DCBs) have emerged as a super important tool in the realm of interventional cardiology, particularly when dealing with restenosis and calcified lesions. The premise behind DCB technology is relatively simple yet brilliant: after aggressive debulking, these balloons deliver an antiproliferative drug directly to the affected area, aiming to reduce the chances of the artery narrowing again.
This method provides several advantages compared to permanent stents. For one, there is no foreign body left behind in the vessel, which minimizes problems related to stent thrombosis and long-term intimal hyperplasia. Moreover, the use of DCBs allows for a more natural healing process, as the artery is able to return to its native state without continuous mechanical irritation. When discussing the finer points of coronary intervention, it is important to note that each of these benefits contributes to a more balanced approach to patient care.
Learning from the Real-World Case: A Discussion on Restenosis Management
Let’s take a closer look at the case at hand. The 76-year-old patient experienced restenosis every six months after his initial PCI procedure. Each recurrence presented a set of swirling, complicated pieces that required an alternative solution to standard stenting methods. The decision to perform repeated stent-free PCI—paired with both aggressive debulking and subsequent treatment with a DCB—was driven by both clinical necessity and a willingness to explore new techniques.
Over time, following three rounds of the combined treatment strategy, the lesion remained free from restenosis for over four years. This real-world evidence suggests that in selected cases, repeated PCI approaches may not only be viable but could offer a lasting solution when conventional methods repeatedly fall short.
Patient-Centered Considerations in Repeated PCI Procedures
From a patient’s perspective, the benefits of a stent-free approach can be quite profound. For individuals who have experienced repeated restenosis, the cumulative impact of multiple interventions can be intimidating and overwhelming. It is essential that all members of the healthcare team—interventional cardiologists, cardiac surgeons, and primary care providers—take these small distinctions into account when planning a patient’s treatment course.
Discussing the procedure in lay terms can help patients better understand what to expect. For example, whereas stents may offer immediate mechanical support, repeated stent-free debulking sessions can gradually decrease the problematic calcification in a way that could eventually lead to fewer repeat procedures and less medication dependency. This patient-centric approach ensures that the treatment plan is not only clinically sound but also empathetic to the patient’s unique journey through coronary care.
The Role of Innovation in Modern Cardiovascular Medicine
This case, along with other emerging evidence, is pushing the boundaries of what is possible in the treatment of coronary artery disease. Innovation in cardiovascular medicine is not limited solely to new devices or drugs; it also encompasses the creative rethinking of treatment strategies. For many, adopting the stent-free approach with repeated debulking and drug-coated balloons might initially seem like threading a needle in a room full of twisting wires. But the progressive nature of cardiovascular diseases demands versatility and adaptability from our treatment protocols.
Continuous learning and adaptation are essential. The new approach challenges the status quo and encourages the medical community to reexamine old ideas in light of new evidence. This sort of evolution in medical practice is not without its risks and uncertainties, which is why it is so critical that robust clinical studies and long-term follow-ups become the cornerstone of any innovative treatment protocol.
Weighing the Benefits and Risks: A Balanced Perspective
While the success in the case of our 76-year-old patient is promising, it is important to maintain a balanced perspective. The benefits of repeated stent-free PCI—such as avoiding the complications linked to a permanent implant—must be carefully weighed against potential risks. Any procedure involving aggressive debulking is not without its inherent challenges, and every patient’s anatomy is subject to slight differences that can dictate the outcome.
Below are some of the key pros and cons observed with this emerging technique:
- Pros:
- No permanent implant, which avoids long-term stent-related complications.
- Targeted drug delivery helps reduce the frequency of future restenosis.
- The approach addresses the trickier parts of calcified lesions by mechanically removing the blockage.
- Potential for improved vessel healing with a more natural restoration of blood flow.
- Cons:
- Repeated procedures can be intimidating and require careful patient monitoring.
- The process of aggressive debulking demands high expertise and may not be suitable for every patient.
- There is still ongoing debate over long-term outcomes for such a strategy.
- Risks of procedural complications, such as vessel injury, must be carefully managed.
Given these points, it is clear that while the repeated stent-free PCI approach offers exciting possibilities, it should be considered only after a careful evaluation of each individual patient’s condition and cardiovascular risk profile.
Understanding the Small Distinctions in Coronary Intervention Strategies
Diving into the subject further, one can see that the small distinctions between various intervention strategies have a huge impact on patient outcomes. Traditional stent implantation provides immediate support to the affected vessel but often leaves behind a foreign body that may incite long-term inflammatory responses. In contrast, a stent-free method that combines aggressive debulking with a DCB not only addresses the immediate obstruction but also minimizes the lingering issues tied to standard metal stents.
It is these little twists in treatment that highlight the beauty—and the challenge—of modern cardiovascular care. Each nuance in these strategies is worth a closer look, because understanding these subtle parts can be the key to improving overall outcomes. The evolution of interventional techniques continues to teach us that sometimes the seemingly off-putting approach can lead to breakthroughs when managed with precision and care.
Lessons Learned: A Four-Year Follow-Up and Beyond
One of the most compelling aspects of this case is the durability of the treatment over a four-year follow-up period. Maintaining a lesion-free state in a patient with a history of repetitive restenosis is no small feat. This longevity suggests that with consistent monitoring and timely intervention, repeated debulking combined with DCB therapy may pave the way for a new standard of care in managing calcified nodules.
Four years is a significant window in the life of a coronary intervention, particularly when many traditional methods show early failures. The sustained success reinforces the belief that interventional cardiologists might have a super important new option at their disposal. As more patients are treated with this method and their outcomes are documented, the medical community may increasingly view the approach as a practical alternative to permanent stenting in select cases.
Taking the Wheel in a Changing Landscape of Cardiovascular Medicine
As the field of cardiovascular medicine continues to experience rapid transformation, healthcare professionals are finding themselves faced with the task of figuring a path through a maze of emerging techniques and technologies. Working through new treatment strategies requires both a willingness to experiment and a commitment to patient safety. The case of repeated stent-free PCI with DCB provides a worthwhile example of how thoughtful innovation can translate into real-world benefits.
The process is similar to steering through a winding road: every twist and turn brings its own set of challenges, but with careful planning and execution, the destination—improved patient outcomes—can be reached. It is also a reminder that a willingness to take calculated risks, when balanced with rigorous clinical evaluation, is a critical element in the advancement of modern medical practice.
Expert Opinions and Future Research Directions
The current debate over the best approach for treating calcified nodules underscores the need for more comprehensive research. While anecdotal cases and smaller studies have demonstrated encouraging results with repeated stent-free PCI, larger randomized controlled trials are essential. Future research should aim to compare this innovative strategy against traditional methods in terms of long-term efficacy, safety, and quality of life outcomes.
Expert opinions in the field are divided, with some arguing that the nerve-racking nature of repeated invasive procedures may dissuade their widespread adoption, while others remain optimistic about the potential benefits. Whether it is the judicious use of aggressive debulking, the precise application of drug-coated technology, or a combination of both, the ongoing dialogue is a clear indication that this strategy is one to watch closely in the years to come.
Some specific areas of future research include:
- Comparative effectiveness studies between repeated stent-free PCI and conventional drug-eluting stent implantation.
- Long-term follow-up studies that track patient outcomes beyond the four-year mark.
- Investigation into the optimal frequency and intensity of debulking procedures required to maintain vessel patency.
- Evaluation of new atherectomy devices and next-generation drug-coated balloons that may further refine this approach.
Embracing Collaboration: A Multi-Disciplinary Approach
In today’s complex medical environment, breakthroughs are rarely the result of isolated efforts. The advancement of techniques such as repeated stent-free PCI with DCB is fundamentally tied to collaboration between various specialties. Cardiologists, interventional radiologists, and cardiovascular surgeons must work together to decide the best course of action for patients facing these tricky conditions.
This collaborative approach not only helps in finding your way through challenging cases but also fosters an environment where different perspectives lead to improved treatment protocols. Sharing real-world experience through multi-center registries, professional societies, and international conferences can accelerate the adoption of promising techniques, while also highlighting the nerve-racking aspects that need further refinement.
A multi-disciplinary strategy is particularly valuable when addressing recurrent restenosis. Each team member brings a unique set of skills to the table—from the fine points of device selection to the subtle parts of patient aftercare—ensuring that the final treatment plan is as holistic as possible. Embracing collaboration can lead to richer insights, smoother patient experiences, and ultimately, better clinical outcomes.
Patient Experiences and the Real-World Impact of Cutting-Edge Techniques
While clinical trials and controlled studies provide critical data, the real measure of success often lies in the patient experience. For individuals with recurrent calcified nodules, the nerve-racking prospect of additional interventions is a genuine concern. Yet, the reported case shows that sometimes, the combination of repeated debulking and DCB treatment can alleviate recurring symptoms and provide sustained relief.
Patients who have undergone these procedures have noted improvements not just in their physical health but also in their overall quality of life. The removal of the repetitive cycle of restenosis can diminish the psychological burden, giving them hope for a more stable future. This human-centric perspective is an essential counterbalance to the technical complexities of the treatment itself.
In patient consultations, it can be very helpful to break down the approach into simple steps:
- Clear explanation of how repeated debulking helps remove the hardened deposits.
- Discussion of the role DCBs play in keeping the vessel open without leaving behind a scar of metal.
- Dialogue around the expected timeline and necessary follow-up visits to monitor the artery’s condition.
- Communication of both the benefits and the nerve-racking aspects of repeated procedures, ensuring that expectations are realistic.
Shaping Future Guidelines and Policy Implications
As methods like repeated stent-free PCI with aggressive debulking and DCB gain traction, it becomes increasingly important to translate emerging clinical evidence into clear guidelines and policy. Regulatory bodies and professional organizations must work in tandem with leading practitioners to establish criteria that ensure patient safety while fostering innovation.
Policy will have to address a variety of questions: How should risks and benefits be weighed in patients with calcified nodules? What best practices can be standardized for patient selection? And how can long-term monitoring be incorporated into treatment protocols? Answering these questions means policymakers, clinicians, and medical device manufacturers must join forces and share their collective insights.
By establishing clear guidelines, the medical community can help steer through the tangled issues of emerging techniques. Furthermore, aligning research priorities with clinical practice will facilitate smoother integration of these methods into everyday practice, ensuring that advancements in care are accessible to all who need them.
Conclusions: A Promising Alternative or a Temporary Fix?
The journey to improve the outcomes for patients with challenging coronary lesions is filled with twists and turns. The case of repeated stent-free PCI for calcified nodules highlights both the promise and the pitfalls of innovative treatment strategies. While the four-year success follows a nerve-racking series of procedures, it nonetheless illustrates an important alternative approach for patients who have seen little success with conventional stenting.
Current evidence suggests that aggressive debulking combined with drug-coated balloon angioplasty can be a super important, albeit unconventional, pathway to reduce recurrent restenosis. The balance of benefits and risks is delicate and demands careful patient selection, clear communication, and ongoing clinical research. As controversies remain and more studies come to light, the evolving field of coronary interventions is set to continue challenging established paradigms.
For healthcare professionals and patients alike, one key takeaway is that the future of cardiovascular treatment might lie in more personalized, adaptable approaches rather than a one-size-fits-all solution. As we continue to figure a path through the complex chronic conditions of coronary artery disease, embracing innovation, collaboration, and rigorous long-term evaluation will be critical. This case reminds us that, sometimes, taking a step back and rethinking traditional strategies may open up a new frontier in patient care.
Final Thoughts: The Road Ahead for Interventional Cardiology
In the ever-evolving world of cardiology, there remains a great deal to learn about managing calcified nodules and preventing recurrent restenosis. Innovation does not come without risk—each new technique brings with it a set of intimidating challenges and a learning curve that can be overwhelming. However, the potential reward is a more refined, patient-specific approach to managing complex coronary conditions.
It is crucial that the cardiology community remains open to change and adaptable in the face of these twisted issues. By investing in research, championing multidisciplinary collaboration, and keeping patient experiences at the forefront, interventional cardiologists can build a more resilient and effective framework for treating coronary artery disease. The evolution of treatments like repeated stent-free PCI holds the promise of transforming how we approach difficult cases—turning what once seemed like insurmountable challenges into manageable steps on the road to recovery.
In conclusion, while the innovative approach of repeated debulking and drug-coated balloon application may not yet be ready to replace traditional methods entirely, it certainly provides a compelling option that warrants further exploration. Continued study and dialogue will be necessary to fully unlock the potential of this groundbreaking strategy. For now, this case stands as a testament to how rethinking traditional approaches can lead to meaningful, lasting improvements in patient care.
As we look to the future, the convergence of advanced technology, better procedural techniques, and the commitment to patient-centered care will define the next chapter in interventional cardiology. It remains our responsibility—both as clinicians and as custodians of patient trust—to keep digging into these challenging bits, exploring every small nuance, and ultimately, enhancing the quality of life for those suffering from coronary artery disease.
Originally Post From https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1674711/full
Read more about this topic at
Novel Stentless Strategy With Perfusion and Drug-Coated …
Stentless Angioplasty: A Revolutionary Approach for …